 |
| Cancer cells dividing [Internet] 2017 Mar 22[Cited 2021 July 08] Available from; https://gfycat.com/jubilantflatbarb |
"He never touched the world”
 |
| David before his marrow transplant, 1983 [Internet] [Cited 2021 June 24 ]Available from;https://www.pbs.org/wgbh/americanexperience/features/bubble-david-vetters-death/ |
☀ David Vetter was born in September 1971 at Texas Children’s Hospital in Houston. David had severe combined immunodeficiency, usually referred to as SCID. From birth, he had no functioning immune system. Any stray germ he picked up, be it from touching another person or breathing normal air, could have been lethal.
Seconds after David first drew breath, he was put inside a sterile plastic bubble where he spent 12 years of his life.
The treatment for SCID was bone-marrow transplants and their ability to build a sound immune system in a child who would lack one. David's sister, Katherine, was the intended donor.
But Katherine’s blood turned out not to be a perfect match.
In October 1983, his doctors tried a new bone marrow technique that did not require a perfect blood match. As had originally been planned, Katherine Vetter was the donor. At first, the procedure seemed to work. The body didn't reject the transplant. (1)
But eventually, David became sick for the first time in his life. It is from Burkitt’s lymphoma.
Burkitt’s lymphoma presents with rapidly enlarging lymph node tumor masses involving the chest and/or the abdomen. It has a high tendency to spread to the central nervous system (brain and spinal cord), and can also involve the liver, spleen, and bone marrow. (2)
On February 22nd David died due to complications from Burkitt’s lymphoma.
After His Death, a question Remained!
From where did David got Burkitt's lymphoma;
☀An autopsy from David revealed that Katherine’s transplanted bone marrow contained traces of a dormant virus, Epstein-Barr, which at that time was not detectable by pre-transplant screening. It was dormant and undetected in Katherine’s marrow. It proved to be a killer, the trigger of cancerous tumors that overwhelmed David’s body.
A cell cycle is a series of events that takes place in a cell as it grows and divides. A cell spends most of its time in what is called interphase, and during this time it grows, replicates its chromosomes, and prepares for cell division. The cell then leaves interphase, undergoes mitosis, and completes its division. (3)
All tumors can be classified as either benign or malignant, and a malignant tumor is cancer. (4)
What causes Carcinogenesis?
Carcinogens are agents or substances, such as radiation or certain chemicals, that induce genetic mutations and/or gene expression deregulation leading to cancer. (4)
Metastatic progression of solid tumors can be divided into five major steps:
Mutations to three major classes of genes involved in controlling cell proliferation and death are at the root of most cancers. These classes are DNA repair genes, oncogenes, and tumor suppressor genes
⬢ DNA repair genes code for proteins whose normal function is to correct errors that arise when cells duplicate their DNA prior to cell division.
⬢ DNA repair genes are active throughout the cell cycle, particularly during G2 after DNA replication and before the chromosomes divide.
⬢ Mutations in DNA repair genes can lead to a failure in repair, which in turn allows subsequent mutations to accumulate. Certain forms of hereditary colon cancer involve defects in DNA repair.
⬢ If the rate of DNA damage exceeds the capacity of the cell to repair it, the accumulation of errors can overwhelm the cell and result in cancer. (6)
⭓ Oncogenes are mutated genes whose PRESENCE can stimulate the development of cancer.
⭓ When oncogenes arise in normal cells, they can contribute to the development of cancer by telling cells to make proteins that stimulate excessive cell growth and division.
☀An autopsy from David revealed that Katherine’s transplanted bone marrow contained traces of a dormant virus, Epstein-Barr, which at that time was not detectable by pre-transplant screening. It was dormant and undetected in Katherine’s marrow. It proved to be a killer, the trigger of cancerous tumors that overwhelmed David’s body.
"Burkitt’s lymphoma, particularly the endemic form that is common in Africa, is associated with the Epstein-Barr Virus (EBV) in nearly 100% of cases. Burkitt’s lymphoma is an aggressive form of lymphoma that affects the B-lymphocytes. In the sporadic forms that occur in Western countries, EBV is present in approximately 30% of cases and in 40% of immunodeficiency-associated cases." (2)
David, The bubble boy who defeats SCID, lose to Cancerous Tumour
What are these Tumors and cancers?
🔅 Throughout the life of a healthy organism, body cells divide, differentiate, and die in a carefully controlled manner.
🔅 To divide, a cell must go through several steps known as the Cell Cycle.
 |
| The Cell Cycle. [Internet] [Cited 2021 July 04 ]Available from; https://www2.le.ac.uk/projects/vgec/highereducation/topics/cellcycle-mitosis-meiosis |
🔅 There are two types of cells in the cell cycle. One types of cell divide slowly or not at all. These cells may exit the G1 phase and enter a resting state called G0. In G0, a cell is not actively preparing to divide, it’s just doing its job. And eventually, die.
🔅 The other type of cells divide rapidly, and in these cases, the daughter cells may immediately undergo another round of cell division. For instance, many cell types in an early embryo divide rapidly, and so do cells in a tumor.
🔅 When the cells of a tissue undergo unusual division that serves no useful function for the host, an abnormal tissue mass called a neoplasm (“new growth”) or tumor (“swelling”) may be created. (3)
|
Benign
Tumor |
Malignant
Tumor (Cancers) |
|
A benign tumor is relatively slow growing |
Malignant Tumor relatively grows faster. |
|
And contains cells that are well differentiated. |
Cells comprising malignant tumors are often poorly differentiated. |
|
Cells are well organized. |
The mass is disorganized |
|
A benign tumor is securely encapsulated such that its cells cannot
break away from the cell mass and enter the blood. |
And encapsulation is rare |
|
Benign tumors do not normally cause death, but if they do, they do
so indirectly by compressing or damaging an adjacent organ. |
These growths are lethal to the host unless they are completely
removed or killed. |
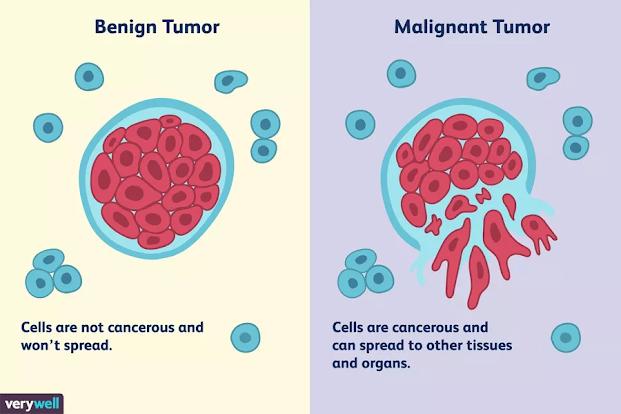 |
| Differences Between a Malignant and Benign Tumor Verywell health [Internet]Lymphoma [Cited 2021 July 04 ]Available from; https://www.verywellhealth.com/what-does-malignant-and-benign-mean-514240 |
How does a normal cell turn into a cancer cell?
★ The transformation of a cell from normal to malignant occurs in a multistep process called carcinogenesis.
★ During carcinogenesis, mutations accumulate in the genes controlling cell proliferation and programmed cell death, resulting in deregulated growth. (4)
★ The process of carcinogenesis may be divided into at least four stages:
★ During carcinogenesis, mutations accumulate in the genes controlling cell proliferation and programmed cell death, resulting in deregulated growth. (4)
★ The process of carcinogenesis may be divided into at least four stages:
Initiation, Promotion, Progression, and Malignant conversion.
👉The initiation
The first stage of carcinogenesis, initiation, results from an irreversible genetic alteration, most likely one or more simple mutations, transversions, transitions, and/or small deletions in DNA.
👉The promotion
The reversible stage of promotion does not involve changes in the structure of DNA but rather in the expression of the genome mediated through promoter-receptor interactions.
If the promoting stimulus is removed, the clone will undergo regression. During the promotion, the target cell is exposed to a stimulus that induces its selective proliferation such that a preneoplastic clone of genetically altered cells develops.
👉The progression
The irreversible stage of progression is characterized by the introduction of additional genetic instabilities that drive the preneoplastic clone to become a neoplastic clone.
Neoplastic clones contain cells that have a significant growth advantage over
normal cells and are on the threshold of malignancy
👉The malignant conversion
Malignant conversion is achieved when a neoplastic cell acquires a transforming mutation that allows invasive growth and confers resistance to normal death signals. (4)
What causes Carcinogenesis?
Carcinogens are agents or substances, such as radiation or certain chemicals, that induce genetic mutations and/or gene expression deregulation leading to cancer. (4)
 |
| Carcinogens [Internet] [Cited 2021 July 08] Available from; https://www.shutterstock.com/image-vector/vector-illustration-carcinogen-icons-set-397920148 |
"Cancer cells have been described as immortal because, unlike normal cells, they don't age and die, but instead can continue to multiply without end."
Can cancer cells spread from their origin?
☄ The spread of cancer cells from the place where they first formed to another part of the body is called Metastasis.
☄ In metastasis, cancer cells break away from the original (primary) tumor, travel through the blood or lymph system, and form a new tumor in other organs or tissues of the body.
The new, metastatic tumor is the same type of cancer as the primary tumor. (5)
For example, if breast cancer spreads to the lung, the cancer cells in the lung are breast cancer cells, not lung cancer cells.
☄Once established and growing in their new locations, these secondary tumors are called metastases.
Metastatic progression of solid tumors can be divided into five major steps:
1) Invasion of the basement membrane and cell migration;
🔻
2) Intravasation into the surrounding vasculature or lymphatic system;
🔻
3) Survival in the circulation;
🔻
4) Extravasation from the vasculature to secondary tissue; and finally,
🔻
5) Colonization at secondary tumor sites (4)
 |
| Metastasis and Angiogenesis [Internet] [Cited 2021 July 08] Available from; https://makeagif.com/gif/metastasis-and-angiogenesis-KhTXcI? |
 |
| Metastasis [Internet] [Cited 2021 July 08] Available from;https://makeagif.com/gif/metastasis-Zjt-_P |
What are the genes that are involved in cancer cell regulation?
Mutations to three major classes of genes involved in controlling cell proliferation and death are at the root of most cancers. These classes are DNA repair genes, oncogenes, and tumor suppressor genes
1)DNA Repair Genes
Correct errors⬢ DNA repair genes code for proteins whose normal function is to correct errors that arise when cells duplicate their DNA prior to cell division.
⬢ DNA repair genes are active throughout the cell cycle, particularly during G2 after DNA replication and before the chromosomes divide.
⬢ Mutations in DNA repair genes can lead to a failure in repair, which in turn allows subsequent mutations to accumulate. Certain forms of hereditary colon cancer involve defects in DNA repair.
 |
| DNA Repair Genes, [Internet] 2013 [Cited 2021 July 06] available from; https://www.mdpi.com/2072-6694/12/8/2315/htm |
⬢ If the rate of DNA damage exceeds the capacity of the cell to repair it, the accumulation of errors can overwhelm the cell and result in cancer. (6)
⬢ A few important DNA repair genes:
BRCA1 and BRCA2
2) Oncogenes
BRCA1 and BRCA2
2) Oncogenes
The bad guys, turn abnormal cell growth on
⭓ An oncogene is a proto-oncogene that has been mutated in a way that leads to signals that cause uncontrolled growth- i.e., cancer.
⭓ An oncogene is a proto-oncogene that has been mutated in a way that leads to signals that cause uncontrolled growth- i.e., cancer.
⭓ Not all genes can mutate and form oncogenes. Only "proto-oncogenes" can mutate to form an oncogene. There are about 70 proto-oncogenes in our DNA.
 |
| Oncogenes [Internet] [Cited 2021 July 07] Available from; https://en.wikipedia.org/wiki/Oncogene |
⭓ Oncogenes are mutated genes whose PRESENCE can stimulate the development of cancer.
⭓ When oncogenes arise in normal cells, they can contribute to the development of cancer by telling cells to make proteins that stimulate excessive cell growth and division.
⭓ Oncogenes are "gain of function" genes. They gain the ability to drive non-stop growth. In spite of their dominant activities, a single mutated oncogene usually isn't enough to cause cancer all by itself because tumor-suppressor genes are acting to put the brakes on to keep cell growth from getting out of control.
 |
| Oncogenes [Internet] 2013 [Cited 2021 July 06] available from; https://www.mdpi.com/2072-6694/12/8/2315/htm |
⭓ Oncogenes aren't usually involved in inherited forms of cancer because most occur as somatic mutations and can't be passed from parent to child. (6)
⭓ A few important oncogenes:
HER-2/neu
HER-2/neu encodes for a cell surface receptor that can stimulate cell division. The HER-2/neu gene is amplified in up to 30% of human breast cancers.
RAS
The Ras gene products are involved in kinase signaling pathways that ultimately control the transcription of genes, regulating cell growth and differentiation.
MYC
The Myc protein is a transcription factor and controls the expression of several genes.
SRC
Src was the first oncogene ever discovered. The Src protein is a tyrosine kinase, which regulates cell activity.
hTERT
hTERT codes for an enzyme (telomerase) that maintains chromosome ends.
HER-2/neu encodes for a cell surface receptor that can stimulate cell division. The HER-2/neu gene is amplified in up to 30% of human breast cancers.
RAS
The Ras gene products are involved in kinase signaling pathways that ultimately control the transcription of genes, regulating cell growth and differentiation.
MYC
The Myc protein is a transcription factor and controls the expression of several genes.
SRC
Src was the first oncogene ever discovered. The Src protein is a tyrosine kinase, which regulates cell activity.
hTERT
hTERT codes for an enzyme (telomerase) that maintains chromosome ends.
 |
Molecular Oncology [Internet] [Cited 2021 July 07] Available from; https://www.rerf.or.jp/en/about/organization-en/chart-e/radi-e/oncog/ |
3) Tumor-Suppressor Genes
The good guys, turn cell growth off
◆ Tumor suppressor genes in normal cells act as braking signals during phase G1 of the cell cycle, to stop or slow the cell cycle before the S phase. If tumor-suppressor genes are mutated, the normal brake mechanism will be disabled, resulting in uncontrolled growth, i.e. cancer.
◆ Tumor suppressor genes in normal cells act as braking signals during phase G1 of the cell cycle, to stop or slow the cell cycle before the S phase. If tumor-suppressor genes are mutated, the normal brake mechanism will be disabled, resulting in uncontrolled growth, i.e. cancer.
 |
What Are Tumor Suppressor Genes? National Cancer Institute (NCI) [Internet] [Cited 2021 July 07] Available from; https://visualsonline.cancer.gov/details.cfm?imageid=12495 |
◆ Mutations in tumor-suppressor genes cause loss of function. Loss-of-function mutations generally only show up when both copies of the gene are mutated. In other words, if a pair of tumor suppressor genes are lost or mutated, their functional absence might allow cancer to develop.
◆ Individuals who inherit an increased risk of developing cancer often are born with one defective copy of a tumor suppressor gene.
◆ Because genes come in pairs (one inherited from each parent), an inherited defect in one copy will not lead to cancer because the other normal copy is still functional. But if the second copy undergoes mutation, the person may develop cancer because there no longer is any functional copy of the gene. (6)
◆ Individuals who inherit an increased risk of developing cancer often are born with one defective copy of a tumor suppressor gene.
◆ Because genes come in pairs (one inherited from each parent), an inherited defect in one copy will not lead to cancer because the other normal copy is still functional. But if the second copy undergoes mutation, the person may develop cancer because there no longer is any functional copy of the gene. (6)
 |
| Tumor-Suppressor Genes [Internet] 2013 [Cited 2021 July 06] available from; https://www.mdpi.com/2072-6694/12/8/2315/htm |
◆ A few important tumor-suppressor genes:
p53: a transcription factor that regulates cell division and cell death.
Rb: alters the activity of transcription factors and therefore controls cell division.
APC: controls the availability of a transcription factor.
One of the main functions of our immune system is Immunosurveillance.
 |
| Introduction to immunology [Internet] [Cited 2021 July 07] available from;https://slideplayer.com/slide/13006713/ |
Immunosurveillance is a term used to describe the processes by which cells of the immune system look for and recognize foreign pathogens, such as bacteria and viruses, or pre-cancerous and cancerous cells in the body.
- Tumor immunosurveillance, regression, and therapy require most often the action of CD8+ T cells.
- These cells are primed by dendritic cells (DC), which are the only antigen-presenting cells able to stimulate naive T cells.
- Tumor antigen presentation requires cross-presentation of antigens from the tumor cells by DC.
- Dendritic cells capture antigens from tumor cells into endosomal compartments and process them.
- Then they expose at their cell surface their own MHC class I molecules complexed with tumor cell epitopes, which are recognized by the T cell receptors of specific CD8+ T cells.
- This allows the activation of anti-tumoral functions of these specific CD8+ T cells, mediated by cytokines and by cytotoxic mechanisms. (7)
 |
| Pathways affecting cytotoxic T lymphocyte activity within the tumor microenvironment |
Nature [Internet] 2017 July 13 [Cited 2021 July 08] Available from; https://www.nature.com/articles/bjc2017220/figures/1
What are the functions of Adaptive immunity and Innate immunity in immunosurveillance?
✤ Experimental and clinical studies indicate that cells of the innate and adaptive immune systems have both anti- and pro-tumor activities.
✤ T cells are a very heterogeneous population: on one hand, CD8 +, CD4 +, and γδT cells are directly involved in the specific killing of tumor cells, directed by the recognition of tumor antigens. On the other hand, regulatory T cells (TRegs) promote the establishment of a pro-tumoral environment
✤ NK cells are also able to induce tumor cell killing based on the detection of activating danger signals on the tumor cell surface, while also secreting pro-inflammatory cytokines
✤ B cells are of major importance for the establishment of anti-tumoral immunity due to their role in antibody production and in the formation of tertiary lymphoid structures in the periphery of the primary tumor, where they also exert the function of presenting antigen to T cells, activating them.
✤ The role of antigen presentation is also performed by dendritic cells, which hold the unique ability to cross-present tumor antigens to CD8 + T cells, promoting direct cell killing. (11)
 |
| How do T cells fight cancer? [Internet] [Cited 2021 July 08] available from; https://gfycat.com/bewitchednervouscockroach |
 |
| Macrophage engulfing a cancer cell [Internet] [Cited 2021 July 08] Available from; https://www.cancerresearch.org/en-us/immunotherapy/treatment-types/targeted-antibodies |
✤ The importance of adaptive immunity for tumor immunosurveillance was first established through studies of mice harboring targeted mutations of the recombinase activating gene-2 (RAG-2), which lack all B lymphocytes, αβ and γδ T cells, and NKT cells.
✤ These mice manifested an increased susceptibility to chemically induced tumors, and the fibrosarcomas arising in these animals were frequently rejected upon transplant to wild-type animals.
✤ Subsequent studies of mice deficient in T cells alone revealed a similar enhanced susceptibility to chemical carcinogens, highlighting the key roles of T lymphocytes in tumor protection.
✤ Consistent with these findings, the development of intra-tumoral T cell infiltrates in multiple cancers is correlated with the absence of early metastasis and prolonged disease-free survival. (8)
⭐The adaptive immune system, however, may also promote carcinogenesis within the background of chronic inflammation. In transgenic models of hepatitis B-induced liver cancer, smoldering CD4+ and CD8+ T-cell responses are required for the progression of hepatocellular carcinoma. Similarly, CD4+ T cells activated by normal cutaneous bacterial flora promote the evolution of squamous cell carcinoma in a human papillomavirus transgenic model. (8)
Tumor antigens are those presented by MHC class I or II molecules on the surface of tumor cells.
How cells in the immune system identify Tumor cells?
 |
| Hitting the Target: How T Cells Detect and Eliminate Tumors Zamora AE,Europe PMC [Internet] 2018 Jan o1 [Cited 2021 July 08] Available from; https://europepmc.org/article/med/29311380 |
Tumor antigens are those presented by MHC class I or II molecules on the surface of tumor cells.
These antigens are sometimes presented only by tumor cells and never by normal cells. In this case, they are called tumor-specific antigens (TSAs) and typically result from a tumor-specific mutation. More common are antigens presented by tumor cells that are called tumor-associated antigens (TAAs). (4)
A TAA of a tumor cell is a normal protein or carbohydrate expressed in a way that is abnormal relative to its status in the healthy, fully differentiated cells in the surrounding tissue of origin.
In other words, a TAA is almost always a case of the “right molecule expressed at the wrong concentration, place and/or time.” (4)
TSAs are new macromolecules that are unique to the tumor and are not produced by any type of normal cell. Because of their non-self nature, TSAs should constitute true immunogens capable of provoking an immune response. However, for reasons that are elaborated in this section, very few of them do. The cancer cells expressing these TSAs, therefore, continue to grow unchallenged. (4)
| Tumor-Specific Antigens | Tumor-Associated Antigens |
|---|---|
| Expressed by tumor cells | Self-antigens expressed by tumor cells |
| Not present in normal host cells | Present in a subset of normal host cells |
| Arise mostly from oncogenic driver mutations that generate novel peptide sequences (i.e. neoantigens) | Arise mostly from genetic amplification or post-translational modifications |
| Can also be generated by oncoviruses | A tendency for expression that is higher and preferential for tumor cells |
| Example: Alpha-fetoprotein (AFP) expression in germ cell tumors and hepatocellular carcinoma | Example: Melanoma-associated antigen (MAGE) expressed in the testis along with malignant melanoma (10) |
How can we know if a person is suffering from cancer?
Sometimes a lump or continuous headache may be Symptoms of cancer... What are the other symptoms?
This can be a little complicated. Because some cancers (pancreatic and liver, in particular) can have few to no symptoms until they’re advanced and difficult to treat, symptoms aren‘t always the best way to find cancer.
 |
| Health Central [Internet] [Cited 2021 July 08] available from;https://www.healthcentral.com/condition/cancer |
What are the treatments for cancer? (9)
Surgery- The goal of surgery is to remove cancer or as much, cancer as possible.
Chemotherapy- Chemotherapy uses drugs to kill cancer cells.
Radiation therapy- Radiation therapy uses high-powered energy beams, such as X-rays or protons, to kill cancer cells. Radiation treatment can come from a machine outside your body (external beam radiation), or it can be placed inside your body (brachytherapy).
Bone marrow transplant- Your bone marrow is the material inside your bones that makes blood cells from blood stem cells. A bone marrow transplant, also knowns as a stem cell transplant can use your own bone marrow stem cells or those from a donor.
A bone marrow transplant allows your doctor to use higher doses of chemotherapy to treat your cancer. It may also be used to replace diseased bone marrow.
Immunotherapy- Immunotherapy, also known as biological therapy, uses your body's immune system to fight cancer. Cancer can survive unchecked in your body because your immune system doesn't recognize it as an intruder. Immunotherapy can help your immune system "see" cancer and attack it.
Hormone therapy- Some types of cancer are fueled by your body's hormones. Examples include breast cancer and prostate cancer. Removing those hormones from the body or blocking their effects may cause the cancer cells to stop growing.
Targeted drug therapy- Targeted drug treatment focuses on specific abnormalities within cancer cells that allow them to survive.
1. American Experience[Internet] USA: WGBH Educational Foundation; David Vetter's Death [Cited 2021 July 04] available from; https://www.pbs.org/wgbh/americanexperience/features/bubble-david-vetters-death/
2. Leukaemia Foundation [Internet] USA: © 2021 Leukaemia Foundation; Burkitt’s lymphoma [Cited 2021 July 04] available from; https://www.leukaemia.org.au/
3. Chow, A. Y. Cell Cycle Control by Oncogenes and Tumor Suppressors: Driving the Transformation of Normal Cells into Cancerous Cells. Nature Education [Internet] (2010)[Cited 2021 July 04] 3(9):7 available from; https://www.nature.com/scitable/topicpage/cell-cycle-control-by-oncogenes-and-tumor-14191459/
3. Khan Acadamy [Internet] India Phases of the cell cycle [Cited 2021 July 05] available from; https://www.khanacademy.org/science/ap-biology/cell-communication-and-cell-cycle/cell-cycle/a/cell-cycle-phases
4. Mak TW. Saunders ME. Jett BD. Primer to The Immune Response 2nd edition. USA: Elsevier; 2014
5. Hapach, L.A., Mosier, J.A., Wang, W. et al. Engineered models to parse apart the metastatic cascade. npj Precis. Onc. 3, 20[Internet] (2019)[Cited 2021 July 05] available from; https://doi.org/10.1038/s41698-019-0092-3
6. Cancer Information and Support Network; Oncogenes, Tumor-Suppressor Genes, and DNA Repair Genes,[Internet] UK; CISA 2013 [Cited 2021 July 06] Available from; https://cisncancer.org/research/what_we_know/advances/oncogenes.html
7. Stephane Isnard, Etienne Hatton, Jean-Baptiste Guillerme, Anne Hosmalin, Chapter Eighteen - Monitoring antigen cross-presentation by human dendritic cells purified from peripheral blood,[internet] Methods in Enzymology, Academic Press, Volume 635,2020,[Cited 2021 July 07] Pages 283-305, Available from; https://doi.org/10.1016/bs.mie.2020.01.004.
(https://www.sciencedirect.com/science/article/pii/S0076687920300264)
8. Kenneth F. May, Masahisa Jinushi, Glenn Dranoff, Chapter 8 - Immunosurveillance: Innate and Adaptive Antitumor Immunity, Cancer Immunotherapy (Second Edition),[Internet] Academic Press, 2013,[Cited 2021 July 07] Pages 101-113, Available from; https://doi.org/10.1016/B978-0-12-394296-8.00008-7.
(https://www.sciencedirect.com/science/article/pii/B9780123942968000087)
9. Mayo Clinic [Internet] Cancer Treatment-Overview; Mayo Foundation for Medical Education and Research (MFMER) [Cited 2021 July 08] Available from; https://www.mayoclinic.org/tests-procedures/cancer-treatment/about/pac-20393344
10. Bourré L., Targeting Tumor-Associated Antigens and Tumor-Specific Antigens,[Internet] Oncology; September 17, 2019, Cited 2021 July 08] Available from; https://blog.crownbio.com/targeting-tumor-associated-antigens-and-tumor-specific-antigens
11. Batalha, Sofia & Ferreira, Sofia & Brito, Catarina. [Internet]. The Peripheral Immune Landscape of Breast Cancer: Clinical Findings and In Vitro Models for Biomarker Discovery. Cancers.(2021) [Cited 2021 July 08] 13. 1305. Available from;10.3390/cancers13061305.








Comments
Post a Comment