 |
| [Internet] [Cited 2021 July 14]Available from; https://gfycat.com/gifs/search/kidney+transplant |
Can heart patients live a little longer?
Is there a way to live life and then "Gift lives"?
The answer is Transplantations,
A transplant is an organ, tissue, or a group of cells removed from one person (the donor) and surgically transplanted into another person (the recipient or host) or moved from one site to another site in the same person.
Transplants – such as a liver transplant – can save lives. They can also restore function to improve quality of life.
The human leukocyte antigen (HLA) system (the major histocompatibility complex [MHC] in humans) is an important part of the immune system and is controlled by genes located on chromosome 6. It encodes cell surface molecules specialized to present antigenic peptides to the T-cell receptor (TCR) on T cells.
MHC molecules that present antigen (Ag) are divided into 2 main classes:
Direct allorecognition is the process by which donor-derived major histocompatibility complex (MHC)-peptide complexes, typically presented by donor-derived ‘passenger’ dendritic cells, are recognized directly by recipient T cells. (7)
👉The strength and vigor with which direct alloimmune responses are elicited may be explained by the fact that all individuals have a high-precursor frequency of T cells specific for allogeneic MHC-peptide complexes. Approximately 0.01 % of the cells in a standard T cell repertoire are capable of responding to a specific foreign peptide presented by a self-MHC molecule. However, 1–10 % of these T cells can engage intact foreign MHC-peptide complexes. (7)
In indirect allorecognition, recipient CD4+ T cells are stimulated by recipient APCs that have acquired peptides derived from proteins (predominantly MHC molecules) of the donor. (8)
Semi-direct Allorecognition
The semi-direct pathway was basically described in which recipient-derived APCs present both acquired, intact allo-MHC-peptide complexes (direct) and allopeptides in the context of self-MHC (indirect).
Transplantations
"The idea is not to live forever, But maybe to help another live a little longer"
Transplants – such as a liver transplant – can save lives. They can also restore function to improve quality of life.
For example, transplanting the cornea is not necessary for life, but can restore sight. (1)
Organs and tissues transplanted
Transplants can be for:
Transplants can be for:
- Organs – heart, kidney, liver, lung, pancreas, stomach, and intestine
- Tissue – cornea, bone, tendon, skin, pancreas islets, heart valves, nerves, and veins
- Cells – bone marrow and stem cells
- Limbs – hands, arms, and feet. (1)
 | ||
|
Ongoing medical advances and research mean new opportunities for innovation in transplant are expanding to include face transplants. (1)
2). Transplant of tissues from an identical twin
3). Transplants from other people
✮ A transplant between two people who are not genetically identical is called an allotransplant and the process is called allotransplantation. Donor organs and tissues can be from people who are living or people who have died because of a significant brain injury or lack of circulation.
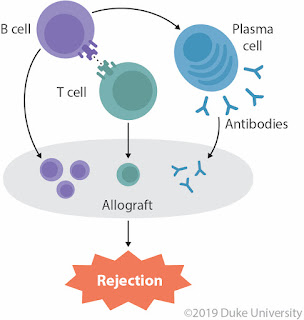
✮ Allotransplantation can create a rejection process where the immune system of the recipient attacks the foreign donor organ or tissue and destroys it. The recipient may need to take immunosuppressive medication for the rest of their life to reduce the risk of rejection of the donated organ.
✮ For some transplants (especially bone marrow), there is also the possibility that immune cells in the donated bone marrow will recognize the host’s body as foreign and attack the cells of the host. This is known as graft-versus-host disease (GvHD). (1)
Initially, the delayed deaths were said to be caused by "secondary disease," which was later renamed graft-versus-host disease (GvHD). GvHD is caused by donor T lymphocytes that destroy recipient cells in the skin, intestinal mucosa, bile ducts, and lymph nodes.
GvHD is opposed by host-versus-graft disease (HvGD), in which host T lymphocytes destroy the administered allogeneic BM cells, including the administered T lymphocytes of the BM donor. (5)
4). Transplants from other species
❇ A transplant between species is called a xenotransplant and the process is called xenotransplantation.
Graft Rejection
Transplantation is a complex area of medicine because when organs or tissues are transplanted from one person to another, the recipient’s immune system can reject and destroy the donor organ or tissue which is called graft rejection, and medication is needed to suppress this immune response. (1)
 |
| Organ transplant ToonsByToons[Internet]2019 Jan 11 [Cited 2021 July 13]Available from; https://www.toonpool.com/cartoons/Organ%20transplant_328428 |
Types of Transplants
 |
| Types of transplants[Internet] [Cited 2021 July 14]Available from; http://repository.limu.edu.ly/bitstream/handle/123456789/404/type%20of%20transplant.pdf?sequence=1&isAllowed=y |
1). Transplants of tissues in the same person
A transplant from one part of your body to another part is called an autograft and the process is called autotransplantation. (3)
👉Some examples of autografts include:
✹ The advantage of an autograft is that the person’s body is unlikely to reject their own cells, so long-term medication to suppress the immune system (immunosuppressants) is not needed.
A transplant from one part of your body to another part is called an autograft and the process is called autotransplantation. (3)
👉Some examples of autografts include:
- Skin graft – uses healthy skin to help heal a wound or burn on another part of the body
- Blood vessel graft – provides an alternative route for blood flow to bypass a blocked artery, for example, in heart bypass surgery
- Bone graft – reconstructs a damaged area of the body, for example, in spinal fusion
- Bone marrow graft – for example, in a person with cancer, bone marrow collected before chemotherapy can replace their blood stem cells after high-dose chemotherapy.
✹ The advantage of an autograft is that the person’s body is unlikely to reject their own cells, so long-term medication to suppress the immune system (immunosuppressants) is not needed.
✹ However, the retrieval (collecting) of the tissue creates a new wound in addition to the transplant site, from which the person will need to recover. (1)
2). Transplant of tissues from an identical twin
✷ Individuals who are syngeneic are identical at all genetic loci, such that transplantation between them may be undertaken without fear of graft rejection. (3)
✷ A transplant between identical twins is called an isograft. The recipient will almost never reject an isograft and so immunosuppressants are not needed.
✷ This is the simplest source of stem cells. Isografts are the least complicated transplants because there is no risk of rejection, graft-versus-host disease (GVHD), or tumor in the marrow.
✷ Blood cell recovery and return of immune system functioning are prompt. The only disadvantage of syngeneic transplants is the lack of the graft versus leukemia (GVL) effect of allogeneic transplants that help reduce tumor relapse.
 |
| [Internet][Cited 2021 July 13] Available from;https://www.pinterest.com/pin/425519864777387799/ |
3). Transplants from other people
✮ A transplant between two people who are not genetically identical is called an allotransplant and the process is called allotransplantation. Donor organs and tissues can be from people who are living or people who have died because of a significant brain injury or lack of circulation.
✮ Allotransplantation can create a rejection process where the immune system of the recipient attacks the foreign donor organ or tissue and destroys it. The recipient may need to take immunosuppressive medication for the rest of their life to reduce the risk of rejection of the donated organ.
✮ For some transplants (especially bone marrow), there is also the possibility that immune cells in the donated bone marrow will recognize the host’s body as foreign and attack the cells of the host. This is known as graft-versus-host disease (GvHD). (1)
Graft vs. Host Diseases (GvHD) and Host vs. Graft Diseases (HvGD)
When considering the history of Bone Marrow Transplant; intravenous administration of allogeneic Bone Marrow cells delayed mortality but did not prevent it.Initially, the delayed deaths were said to be caused by "secondary disease," which was later renamed graft-versus-host disease (GvHD). GvHD is caused by donor T lymphocytes that destroy recipient cells in the skin, intestinal mucosa, bile ducts, and lymph nodes.
GvHD is opposed by host-versus-graft disease (HvGD), in which host T lymphocytes destroy the administered allogeneic BM cells, including the administered T lymphocytes of the BM donor. (5)
4). Transplants from other species
❇ A transplant between species is called a xenotransplant and the process is called xenotransplantation.
❇ Heart valves from cows and pigs have been used for many years to replace faulty heart valves in people.
❇ The animal valves are treated before use to reduce the risk of the immune system rejecting the valve. Heart valves may also be replaced with human valves (allotransplant) or mechanical heart valves. (1)
 | ||
|
The Molecular Basis of Graft Rejection
The ability of immune cells to distinguish between ‘self’ and ‘non-self’ is of fundamental importance. It ensures that invading pathogens are efficiently removed whilst tolerance towards cells of self-origin is maintained.
★ In transplantation, the introduction of ‘non-self’ cells or tissues into a recipient can trigger an immune response. This is initiated when antigens derived from a genetically distinguishable member of the same species are recognized as foreign, a process termed ‘allorecognition’. (6)
Major Histocompatibility Complex (MHC) is the Antigen the immune cells of the recipient identify.
The human leukocyte antigen (HLA) system (the major histocompatibility complex [MHC] in humans) is an important part of the immune system and is controlled by genes located on chromosome 6. It encodes cell surface molecules specialized to present antigenic peptides to the T-cell receptor (TCR) on T cells.
MHC molecules that present antigen (Ag) are divided into 2 main classes:
- Class I MHC molecules
- Class II MHC molecules
The MHC class I and II molecules are the most immunogenic antigens that are recognized during the rejection of an allogeneic transplant. (4)
Immune Recognition of Allogeneic MHC Molecules
How does an allogeneic MHC molecule (allo-MHC) in a graft provoke lymphocyte responses?
For B cells, the mechanism of allo-MHC recognition is straightforward. The allo-MHC molecules of the donor often have a slightly different conformation than recipient MHC molecules, so that the recipient has B cells with BCRs that recognize allo-MHC as they would any incoming non-self protein.
The recipient’s B cells are activated and produce alloantibodies directed against the allo-MHC molecules displayed on the graft surface. (6)
For T cells, the situation is more complex because TCRs recognize epitopes composed of peptides bound to MHC. There are two mechanisms that account
for T cell responses to allo-MHC: direct allorecognition, indirect allorecognition, (6) and Semi-direct allorecognition
Direct allorecognition
Mechanism;
✱ The mechanism focuses on the contribution of the allopeptide bound in the groove of the allo-MHC. ✱ It is believed that specific structural components of self-MHC molecules are ‘mimicked’ by allo-MHC molecules.
✱ As such, self-restricted T cells dock and make contacts with allo-MHC molecules in the same manner as they would with self-MHC molecules.
✱ However, the binding groove of the self-and allo-MHC molecules is vastly different, thus the peptides presented by each are significantly different, despite being derived from similar endogenous proteins.
👉The strength and vigor with which direct alloimmune responses are elicited may be explained by the fact that all individuals have a high-precursor frequency of T cells specific for allogeneic MHC-peptide complexes. Approximately 0.01 % of the cells in a standard T cell repertoire are capable of responding to a specific foreign peptide presented by a self-MHC molecule. However, 1–10 % of these T cells can engage intact foreign MHC-peptide complexes. (7)
Indirect Allorecognition
Mechanism;
✤ When cells of an allogeneic graft die, some of their component proteins are shed into recipient tissues and are taken up by recipient APCs, or recipient APCs may enter the graft itself.
✤ Again, most of these donor proteins are encoded by genes that are monomorphic within a species, so that peptides of these donor proteins are seen as “self.”
✤ If acquired by recipient APCs, these self-peptides are presented on self-MHC and do not provoke an immune response because T cells recognizing this combination were deleted during the establishment of central tolerance.
✤ However, because the MHC molecules of the recipient and donor are usually different, nonself-peptides derived from donor MHC molecules will be generated.
If these peptides are acquired by recipient APCs, they are presented on self-MHC as nonself (self-MHC + X), and an immune response against them is mounted. (8)
✤ Because donor proteins are taken up exogenously, the processing of allo-MHC molecules leads to a presentation by recipient MHC class II molecules and activation of CD4+ T cells. The activated CD4+ T cells secrete cytokines that damage the graft and support the activation of B cells producing alloantibodies directed against the donor protein in the graft.
👉 Indirect allorecognition by CD8+ T cells may also occur due to the cross-presentation of exogenous donor MHC peptides on MHC class I of recipient APC. CD8+ T cells activated in this way can mediate cytotoxicity and express damaging cytokines that contribute to graft rejection. (8)
Differences between Direct and Indirect allorecognition
Semi-direct Allorecognition
The semi-direct pathway was basically described in which recipient-derived APCs present both acquired, intact allo-MHC-peptide complexes (direct) and allopeptides in the context of self-MHC (indirect).
 |
| Semi-direct allorecognition Alherbish A. [Internet] 2006 [Cited 2021 July 15]Available from; https://slideplayer.com/slide/14910658/ |
Mechanism;
✷ The third pathway of recognition also involves donor APCs, but in this case, are their membrane components fused with recipient APCs and therefore can present intact donor MHC molecules to the host. ✷ There are several possibilities how this can be achieved: cell-cell contact (trogocytosis), nanotubes, or release of extracellular vesicles such as exosomes.
✷ Myeloid antigen-presenting cells and dendritic cells in particular are one of the major exosome producers. There are known especially for their ability to transport functional MHC molecules with bonded antigen peptide (pMHC) to different cells population including other dendritic cells.
✷ In consequence, these dendritic cells which acquired new pMHC, displayed on their surface, became “cross-dressed”.
✷ This pMHC is capable of normal antigen presentation to effectors' cells. Usually, the mechanism of cross-dressing serves the purposes of amplifying the immune response to certain antigens, but in the case of alloantigen recognition the APCs are able, thanks to this mechanism, to prime both direct and indirect T lymphocytes by expressing both self- MHC and allo- MHC peptides derived from donor passenger APCs.
👉Semi-direct alloantigen recognition, therefore, contributes to acute rejection by eliciting a response of specialized CD4+ and CD8+ T lymphocytes.
How does allo-MHC in a grafted tissue such as a kidney manage to activate cross-reactive T cells, since naïve T cells are usually activated only in lymph nodes?
☗ Finally, it is possible that chronic inflammation and NK cell activation at the graft site associated with the pro-inflammatory cytokine release and donor cell cytotoxicity can lead to the presentation of formerly sequestered tissue-specific antigens and the processing of cryptic self-determinants. ⧫ During transplantation, donor DCs expressing allo-MHC travel along with the donated organ and are introduced into the recipient.
⧫ These donor DCs can migrate out of the graft into the recipient lymph node draining the transplant site.
⧫ Naïve recipient Th and Tc cells expressing cross-reactive TCRs can then be activated by donor DCs within the node and generate T cell effectors as well as memory T cells.
⧫ The Th effectors support the activation of antigraft B cells and Tc cells within the lymph node, and the differentiated progeny of these cells home back to the graft and attack it. (6)
Natural killer cells in the rejection of solid organ allografts
☗ NK cells can contribute to both acute and chronic allograft rejection by killing directly allogeneic target cells thereby amplifying the inflammatory process and presumably the presentation of allodeterminants to T cells activated in an indirect fashion.
☗ In addition, NK cells can contribute to the rejection process by secreting chemokines necessary for graft infiltration by others and by producing γIFN thus enhancing direct Th1 cell alloreactivity while antagonizing regulatory type immunity.
👉This process may result in chronic allograft rejection mediated essentially by CD4+ autoreactive Th1 cells.
 |
| Innate immune responses in allotransplantation. LaRosa D.F.[Internet] 2007 June 15[Cited 2021 July 13] Available from; https://www.jimmunol.org/content/jimmunol/178/12/7503/F1.large.jpg |
Minimizing Graft Rejection
I. HLA Typing
◉ In order to minimize the intensity of a transplant recipient’s adaptive response to a donated organ, clinicians attempt to ensure the closest possible match between the MHC alleles of the recipient and those of the donor.
◉ Thus, the first step in a transplantation protocol is to determine the MHC haplotype of the prospective recipient. Since MHC molecules in humans are known as HLAs (human leukocyte antigens), this procedure is known as HLA typing. (6)
II. Alloantibody Analysis
i) Alloantibody Screening
Transplant survival is greatly decreased if the recipient has circulating pre-formed alloantibodies that could potentially mediate HAR. Prior alloantibody screening can determine whether anti-HLA antibodies are present in the recipient’s serum and allow the physician to select the donor accordingly.
ii) Cross-Matching
Once a potential donor is identified for a given prospective transplant recipient, a cross-matching test is carried out to confirm that the recipient does not possess any pre-formed antibodies that could attack a graft from that particular donor. A CDC assay can be helpful in this context since it is a functional test that can predict the fate of the cells in a graft.
T cells and B cells are separately isolated from the blood of a prospective donor to enable testing for recipient antibodies against donor MHC class I and class II molecules, respectively.
III. Immunosuppressants
◉ Immunosuppressant, any agent in a class of drugs that is capable of inhibiting the immune system. Immunosuppressants are used primarily to prevent the rejection of an organ following transplantation.
◉ Calcineurin inhibitors are the most effective immunosuppressive drugs in use. These drugs target intracellular signaling pathways induced by the activation of T lymphocytes (or T cells), a type of white blood cell that directly attacks and eliminates foreign molecules from the body. (2)
ii) Cross-Matching
Once a potential donor is identified for a given prospective transplant recipient, a cross-matching test is carried out to confirm that the recipient does not possess any pre-formed antibodies that could attack a graft from that particular donor. A CDC assay can be helpful in this context since it is a functional test that can predict the fate of the cells in a graft.
T cells and B cells are separately isolated from the blood of a prospective donor to enable testing for recipient antibodies against donor MHC class I and class II molecules, respectively.
III. Immunosuppressants
◉ Immunosuppressant, any agent in a class of drugs that is capable of inhibiting the immune system. Immunosuppressants are used primarily to prevent the rejection of an organ following transplantation.
◉ Calcineurin inhibitors are the most effective immunosuppressive drugs in use. These drugs target intracellular signaling pathways induced by the activation of T lymphocytes (or T cells), a type of white blood cell that directly attacks and eliminates foreign molecules from the body. (2)
 |
| Immunosuppressants [Internet][Cited 2021 July 15] Available from; https://www.shutterstock.com/g/tozzi.marta?searchterm=immunosuppressants |
1. Organ and Tissue Transplantation [Internet] Australia; Department of Health, State Government of Victoria, Australia [Reviwed on 2019 Oct. 23] [Cited 2021 July 13] Available from; https://www.betterhealth.vic.gov.au/health/ConditionsAndTreatments/organ-and-tissue-transplantation#bhc-content
2. Britannica, The Editors of Encyclopaedia. "Immunosuppressant". [Internet]Encyclopedia Britannica, 27 Jun. 2018, [Cited 2021 July 15] Available from; https://www.britannica.com/science/immunosuppressant.
3. Types of Bone Marrow Transplants [Internet] Johns Hopkins University & Medicine [Updated 2019 Jan. 28] [Cited 2021 July 13] Available from; https://www.hopkinsmedicine.org/kimmel_cancer_center/cancers_we_treat/bone_marrow_transplant/types_transplants.html
4. Delves P.J., Human Leukocyte Antigen (HLA) System,[Internet] USA; Merck Sharp & Dohme Corp., a subsidiary of Merck & Co., Inc., Kenilworth, NJ, Reviewed 2020 Apr. [Cited 2021 July 14] Available from; https://www.msdmanuals.com/professional/immunology-allergic-disorders/biology-of-the-immune-system/human-leukocyte-antigen-hla-system
5. Vriesendorp HM, Heidt PJ. History of graft-versus-host disease. Exp Hematol.[Internet] 2016 Aug; [Cited 2021 July 14] 44(8):674-88. Available from; DOI: 10.1016/j.exphem.2016.05.011. Epub 2016 May 26. PMID: 27235758.
6. Mak TW. Saunders ME. Jett BD. Primer to The Immune Response 2nd edition. USA: Elsevier; 2014
7. Boardman, D. A., Jacob, J., Smyth, L. A., et al. What Is Direct Allorecognition?. Current transplantation reports [Internet] ,2016 [Cited 2021 July 14]3(4), 275–283. Available from; https://doi.org/10.1007/s40472-016-0115-8
8. Tak W. Mak, Mary E. Saunders,27 - Transplantation, The Immune Response, Academic Press,[Internet] 2006,[Cited 2021 July 14]Pages 873-921, ISBN 9780120884513, Available from; https://doi.org/10.1016/B978-012088451-3.50029-6(https://www.sciencedirect.com/science/article/pii/B9780120884513500296)
9. Benichou, G., Yamada, Y., Aoyama, A., et al. Natural killer cells in rejection and tolerance of solid organ allografts. Current opinion in organ transplantation,[Internet] 2011 [Cited 2021 July 14] 16(1), 47–53. Available from; https://doi.org/10.1097/MOT.0b013e32834254cf
10. Alloantigen recognition.[Internet] 2020 June 22 [Cited 2021 July 14] Available from; https://en.wikipedia.org/wiki/Alloantigen_recognition









Comments
Post a Comment